A Florida advance directive is a set of declarations given to medical professionals on behalf of a patient who may be unable to make decisions about their treatment during the time of care. The State of Florida recognizes a Living Will Declaration, outlining a patient’s wishes, a Designation of Health Care Surrogate, which appoints a third party to make health care decisions on behalf of the patient, and more recently, Physician Orders for Life-Sustaining Treatment (POLST), which provides medical providers with additional direction for care in times of a medical crisis.
Spanish (Español) Version – Adobe PDF
Signing Requirements (§ 765.202(1)) – (2) Two witnesses are required, one of which cannot be the surrogate. At least one witness cannot be a spouse or blood relative.
(a) A witnessed document in writing, voluntarily executed by the principal in accordance with 765.302; or
(b) A witnessed oral statement made by the principal expressing the principal’s instructions concerning life-prolonging procedures.
Florida AARP
Cleveland Clinic
Honoring Choices
USF Advance Directive
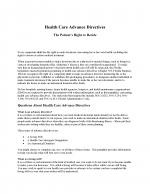
(1) Declaration Date. It will be important to future Reviewers to quickly identify when this document was made upon inspection. This will aid Florida Medical Personnel to see if the declarations made here are the most recent.
(2) Declarant Name. As the potential Florida Patient issuing his or her medical instructions, your name must be presented as the author of the declaration being completed.
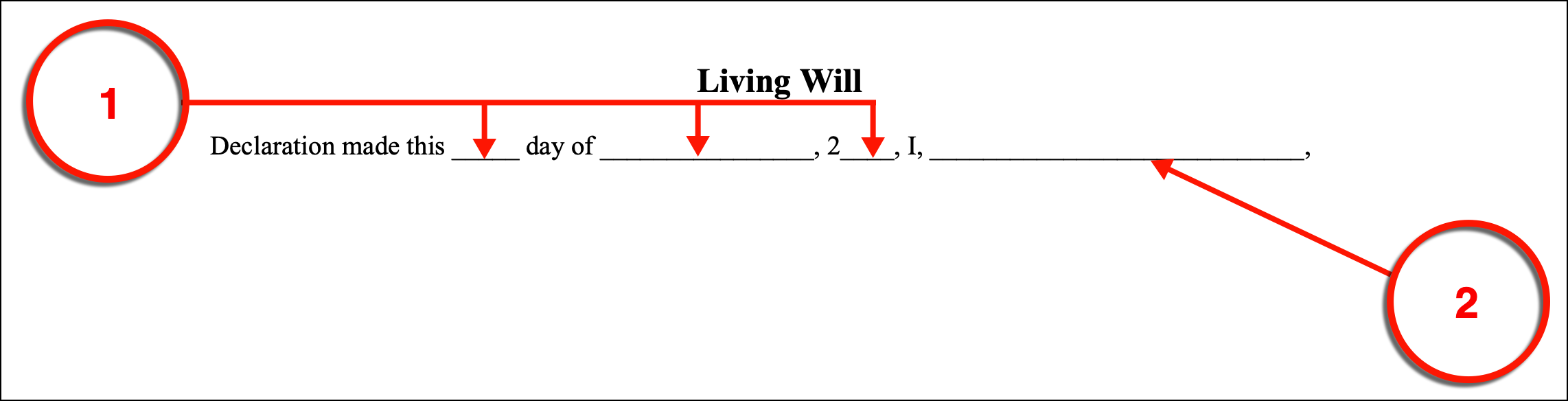
(3) Medical Condition. Any Florida Physician or Medical Personnel reviewing this directive should be kept well-informed which medical condition(s) you wish this directive applied to. You can apply the directives set forth here to go in effect if you have a terminal condition, an end-stage condition, or if you are in a persistent vegetative state by providing your initials where requested.
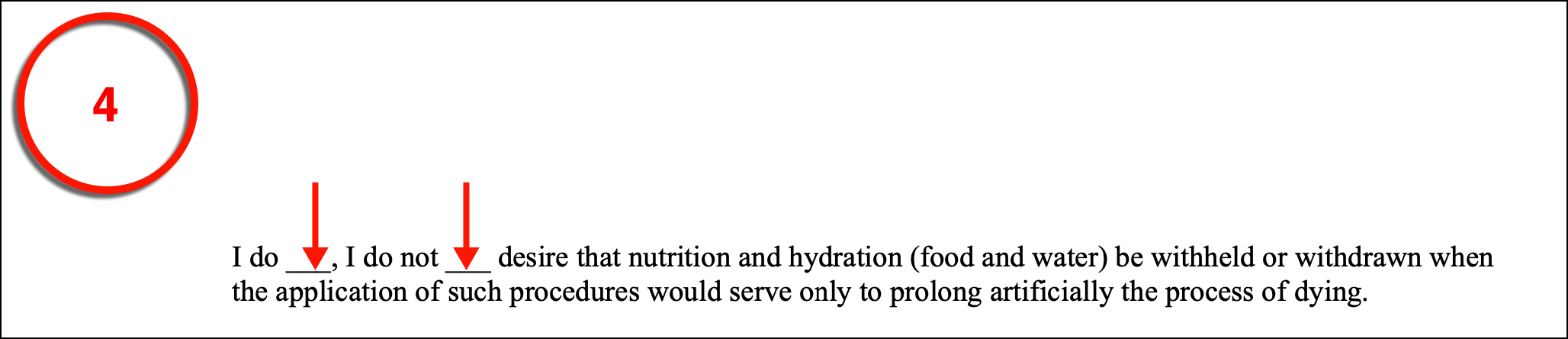
(4) Nutrition And Hydration. If you have been incapacitated and suffering from one or more of the conditions that should prompt this document to be effective then, in many cases, you may become unable to feed yourself or drink fluids. You can provide advance consent or refusal to Florida Physicians seeking to provide you with nutrients and fluids through a tube or I.V. (intravenously) or you can withdraw any such consent by selecting the appropriate phrase from the artificial nutrition statement provided.
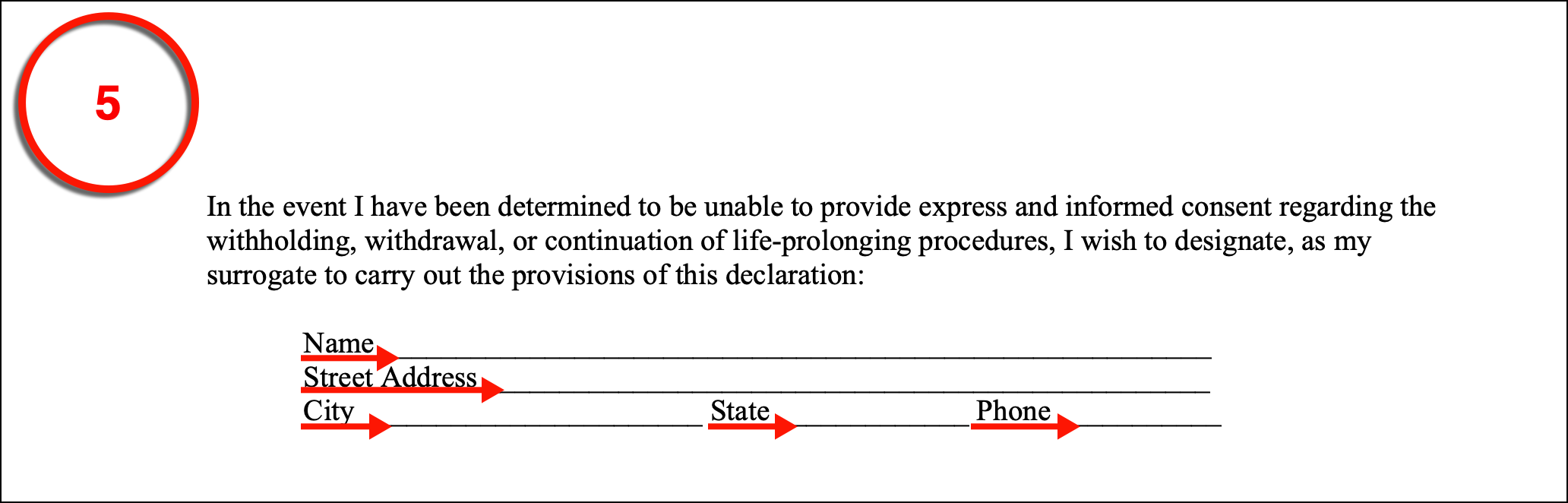
(5) Surrogate Agent. You can inform Florida Physicians that they may seek direction regarding your medical treatment by consulting with a Surrogate Health Care Agent that you name in this form. In addition to his or her name, the Surrogate Health Care Agent should also be identified with his or her address and current phone number.
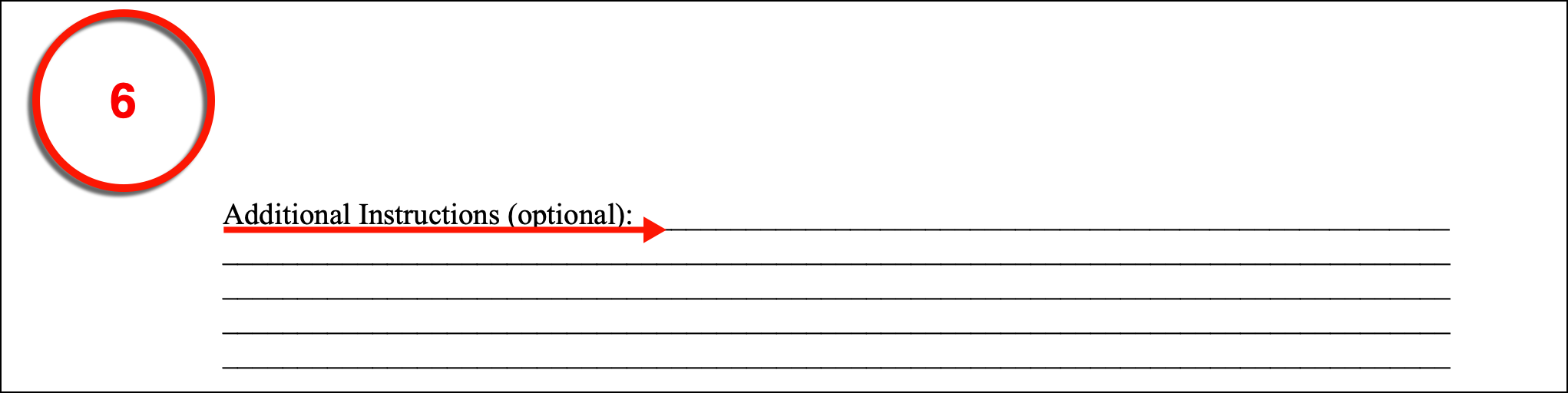
(6) Additional Declarant Instructions. While several statements concerning your medical treatment in Florida should you be unable to communicate and suffering a serious medical condition have been documented within this paperwork, you can add your own instructions for medical care for Florida Medical Providers to follow so long as your requests are legal. This is an optional area, but should you decide to employ this option, make sure all your instructions, restrictions, preferences, and consents are provided before you sign your name. If you require additional space to work, you can continue with an attachment but name the attachment then cite its title in this form.
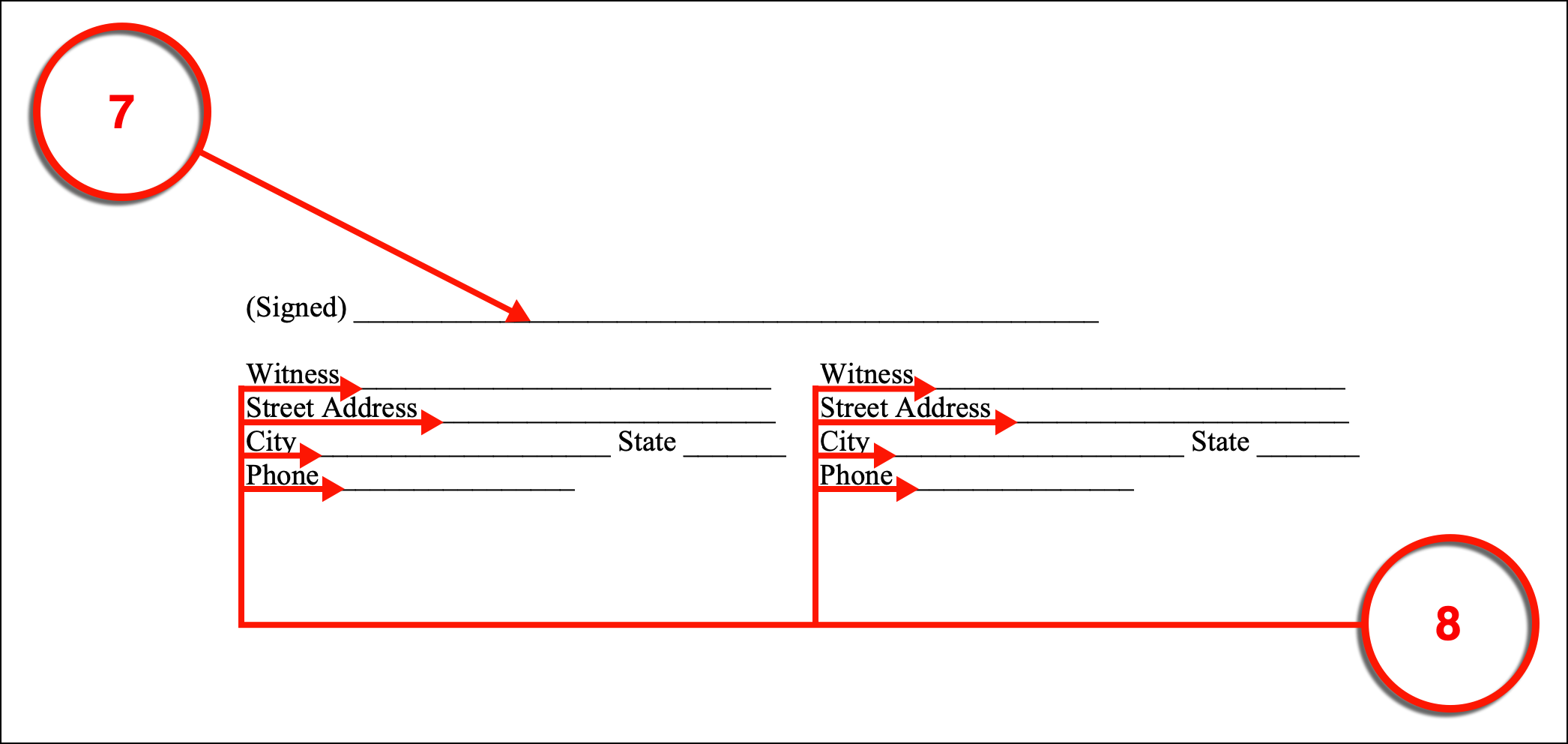
(7) Witnessed Declarant Signature. Your signature as the Florida Declarant is mandatory for this document to be issued. Additionally, two Witnesses must watch you complete this action. Thus, sign your name to complete this form.
(8) Witness Testimonial Signatures. Two Witnesses, one of which may not be related to you, must sign their names to this document after you have provided your name. Each Witness must also accompany the signature provided with his or her address and telephone number.
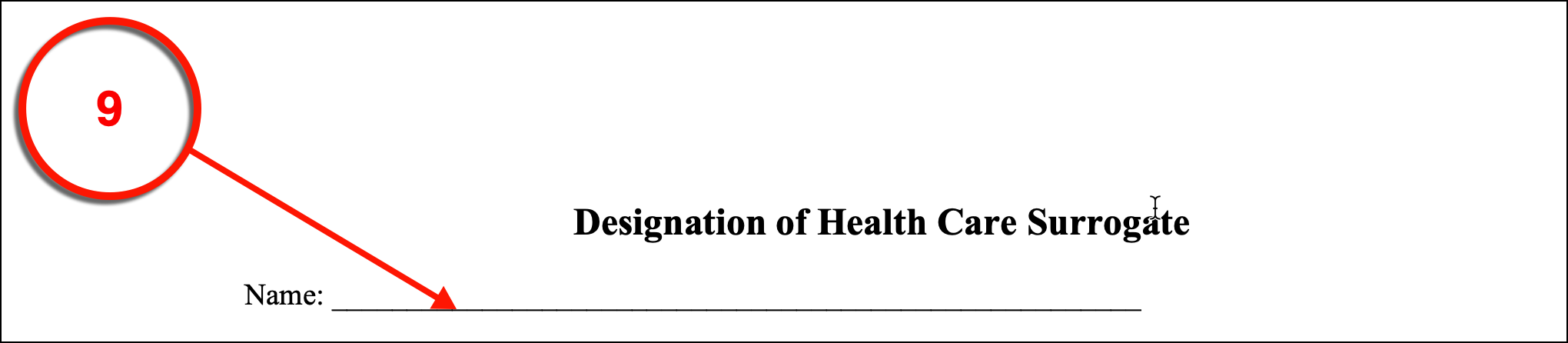
(9) Florida Principal Identity. The next portion of this directive allows a Florida Health Care Surrogate to be given the power to voice your treatment preferences to attending Physicians. Before naming this Party, you must claim the role of the Florida Principal making this appointment by presenting your full name with the title.
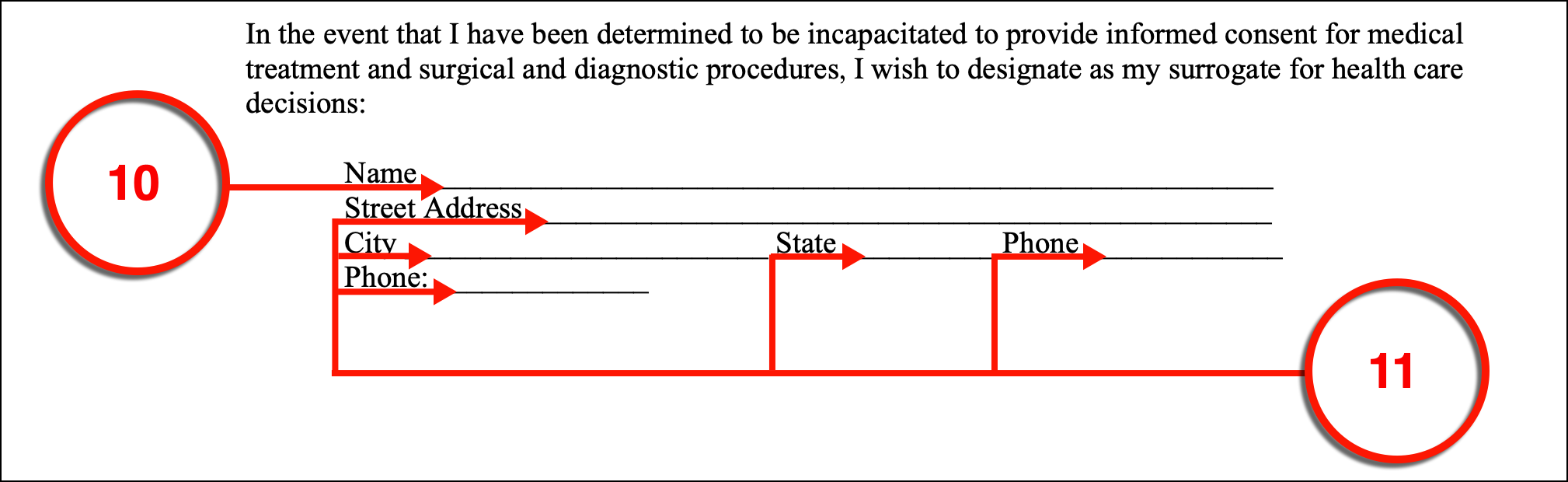
(10) Health Care Surrogate. The full name of the Person you wish Florida Medical Personnel to consult with regarding your treatment preferences should be produced.
(11) Health Care Surrogate Contact Details. The address and phone number where the Florida Health Care Surrogate can be reliably reached is required.
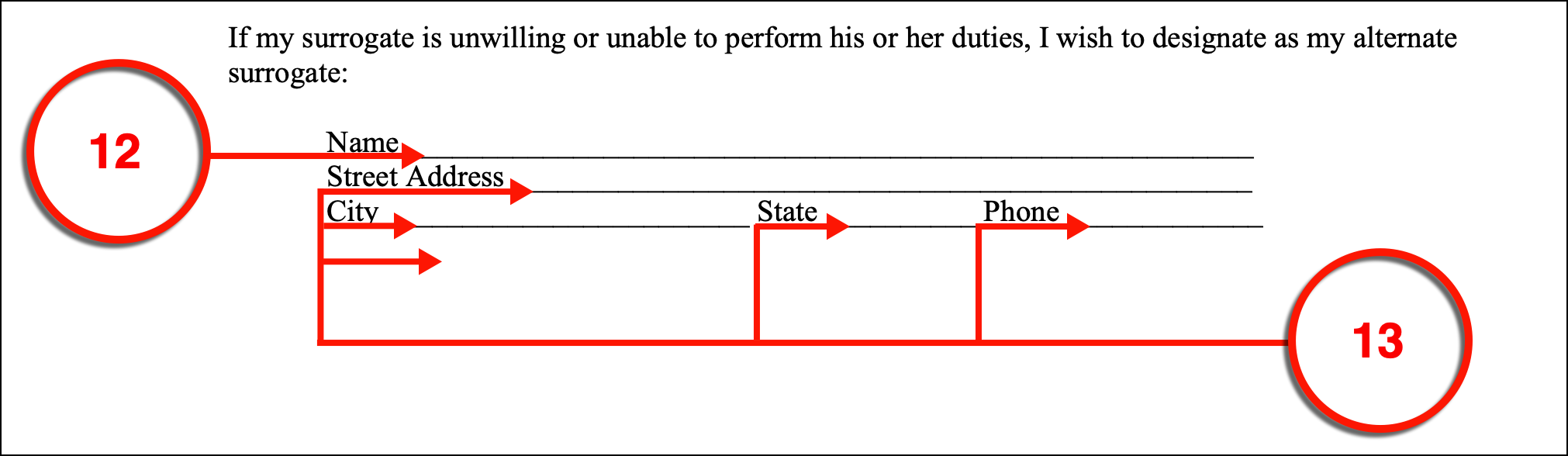
(12) Alternate Surrogate Agent. If the original Health Care Surrogate is not able to represent your wishes to Florida Medical Personnel, has had his or her power revoked, or is unwilling to act in this role when you are unable to communicate then you will not have the representation you counted on. This can leave you extremely vulnerable. To prevent this lack of communication, you can appoint an Alternate Agent to step into the Health Care Surrogate role with the principal authority this document conveys. It should be mentioned this Alternate Surrogate has no ability to make medical decisions in your name unless your original choice has been revoked, is unwilling to convey your medical decisions, or unable to.
(13) Alternate Surrogate Agent Contact Information. It should be considered imperative that your Alternate Health Care Surrogate’s current address and telephone number are recorded accurately.
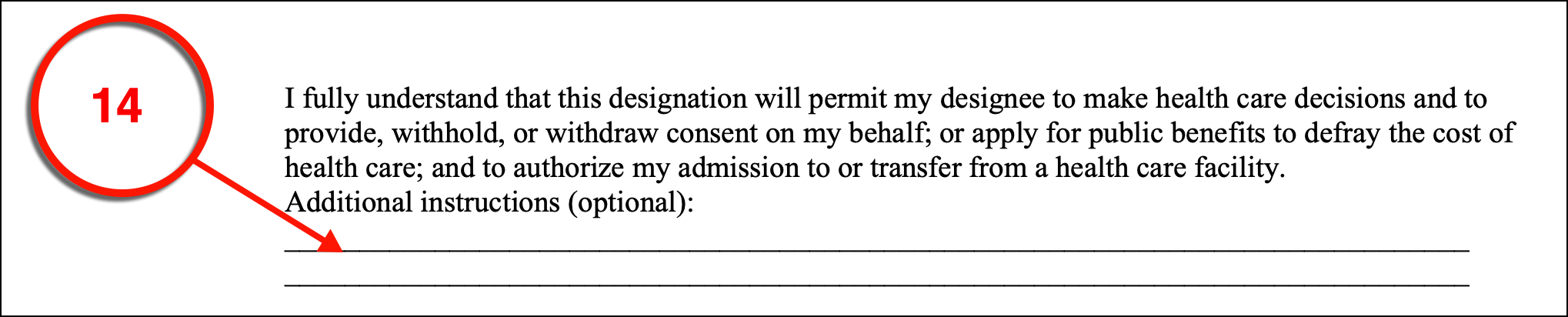
(14) Additional Principal Treatment Directives. There may be medical issues or treatment decisions that you prefer to discuss directly with Florida Health Care Providers and Medical Personnel rather than leaving these topics up to your Surrogate. Use the area provided to include your medical instructions and treatment directives to Florida Care Providers. This is optional but suggested.
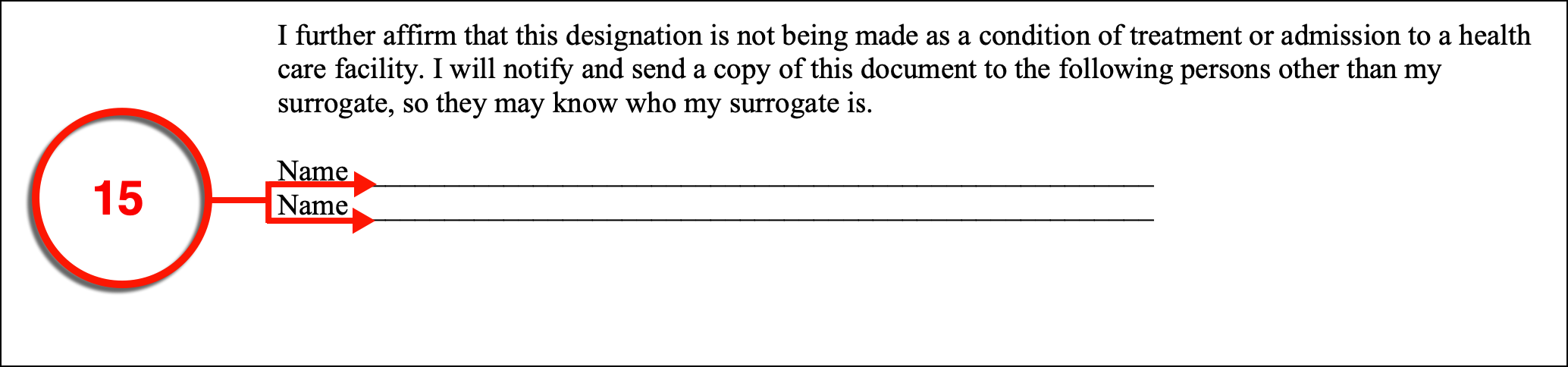
(15) Concerned Parties. Generally, many would consider it wise to make sure that your family members and significant other be aware of this appointment. Therefore, once you have issued your directive, each of these Parties should be provided with a copy. List the name and contact information of each Party you will send a copy of this paperwork to.
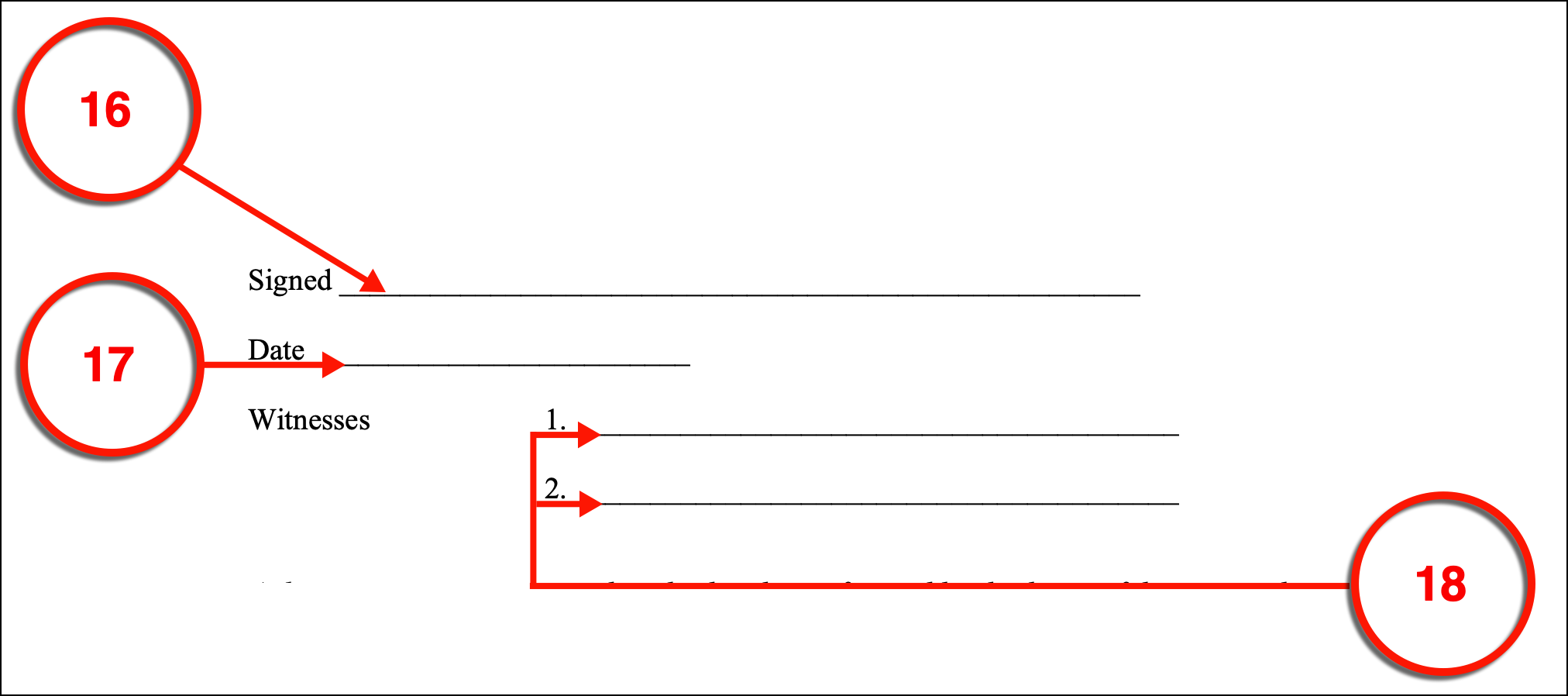
(16) Signature Of Florida Principal. Sign this document before two Witnesses.
(17) Date Of Signing.
(18) Qualified Witness Signatures. Each Witness must provide his or her signature once they have observed your act of signing. Be advised at least one of these Witnesses cannot be related to the Florida Declarant (You) by blood or marriage.
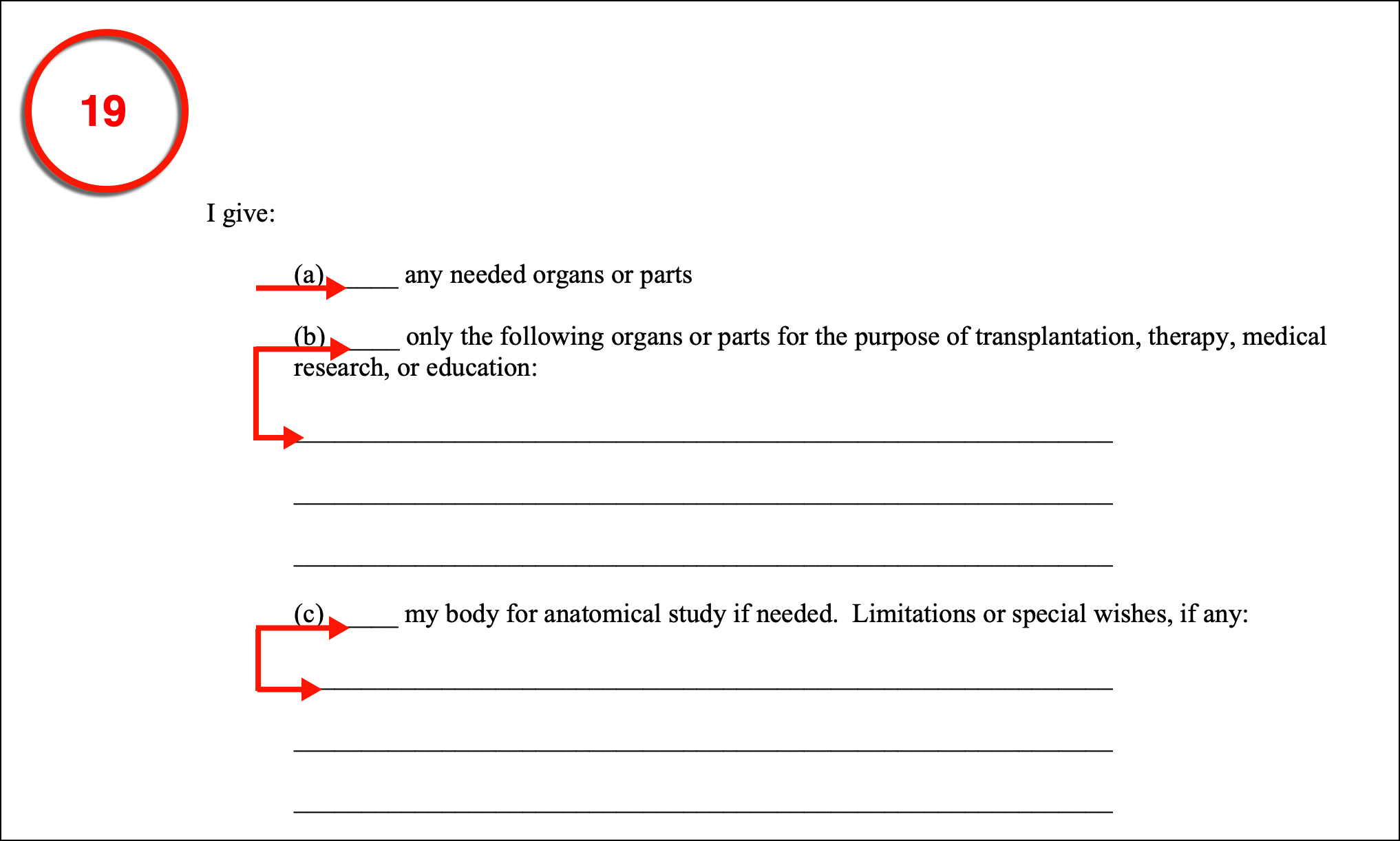
(19) Approved Anatomical Gifts. If desired, you can issue your intent to make anatomical donations through this paperwork by simply initialing the appropriate statement. Be advised that once you initial any of the statements in the donor paperwork provided, it will be assumed that you consent to make the anatomical gifts you discuss here (although, you can always rescind your decision by issuing another directive in the future). Once you have determined the level of donation you would like to make upon death, initial statement A to indicate that any organs or body parts can be donated, statement B to indicate that only organs and tissues you list in this section can be donated, or initial statement C to donate your body for anatomical study while observing any limitations you discuss in this final option. If you do not initial any of these options it will be assumed that you do not consent to make an organ donation.
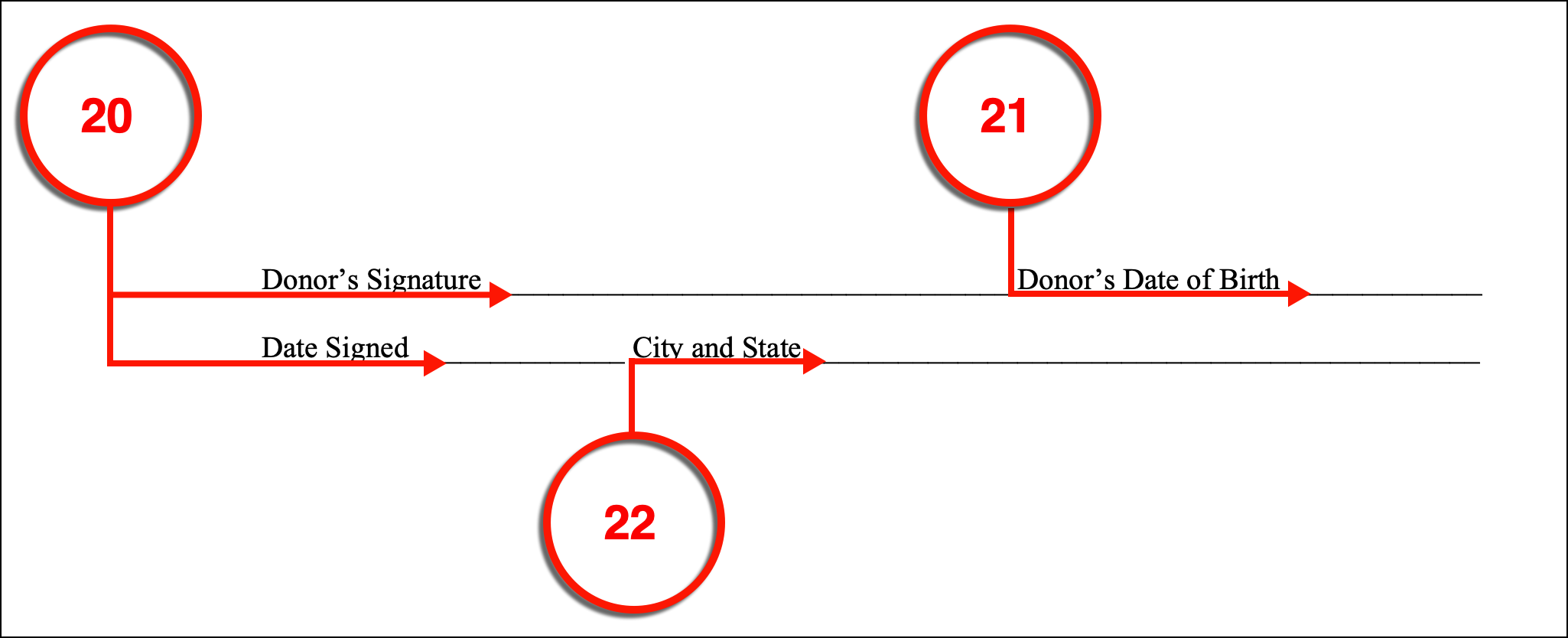
(20) Florida Donor Dated Signature. As the Florida Organ Donor, you must approve this optional form’s inclusion to your directive after it has been completed by signing your name and providing the current date.
(21) Donor’s Date Of Birth. Support your identity by documenting your date of birth.
(22) City And State Of Signing. Produce the city and state where this intent is made.
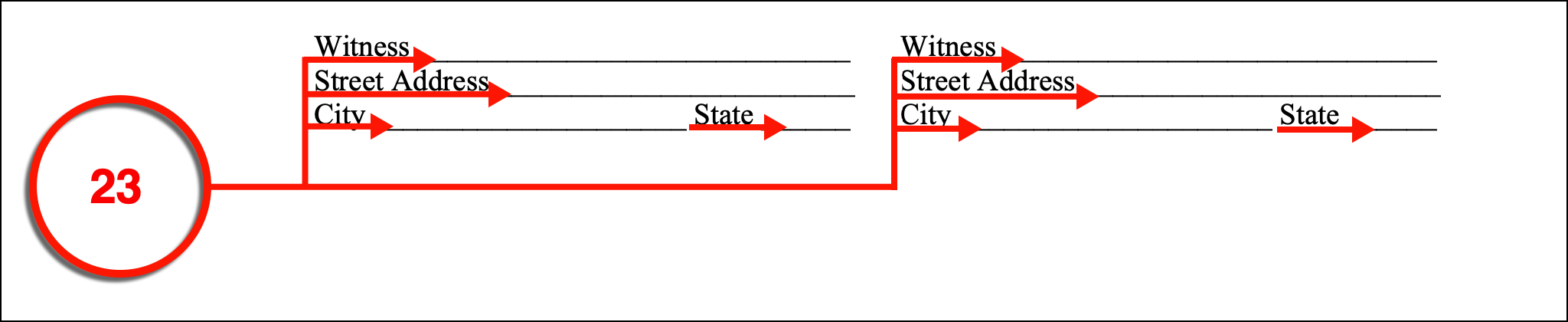
(23) Witness Signature And Address. Two Witnesses will be needed to prove that your act of signing has been an honest action that you performed as they watched. Their signatures and addresses will need to be supplied to make this testimony.
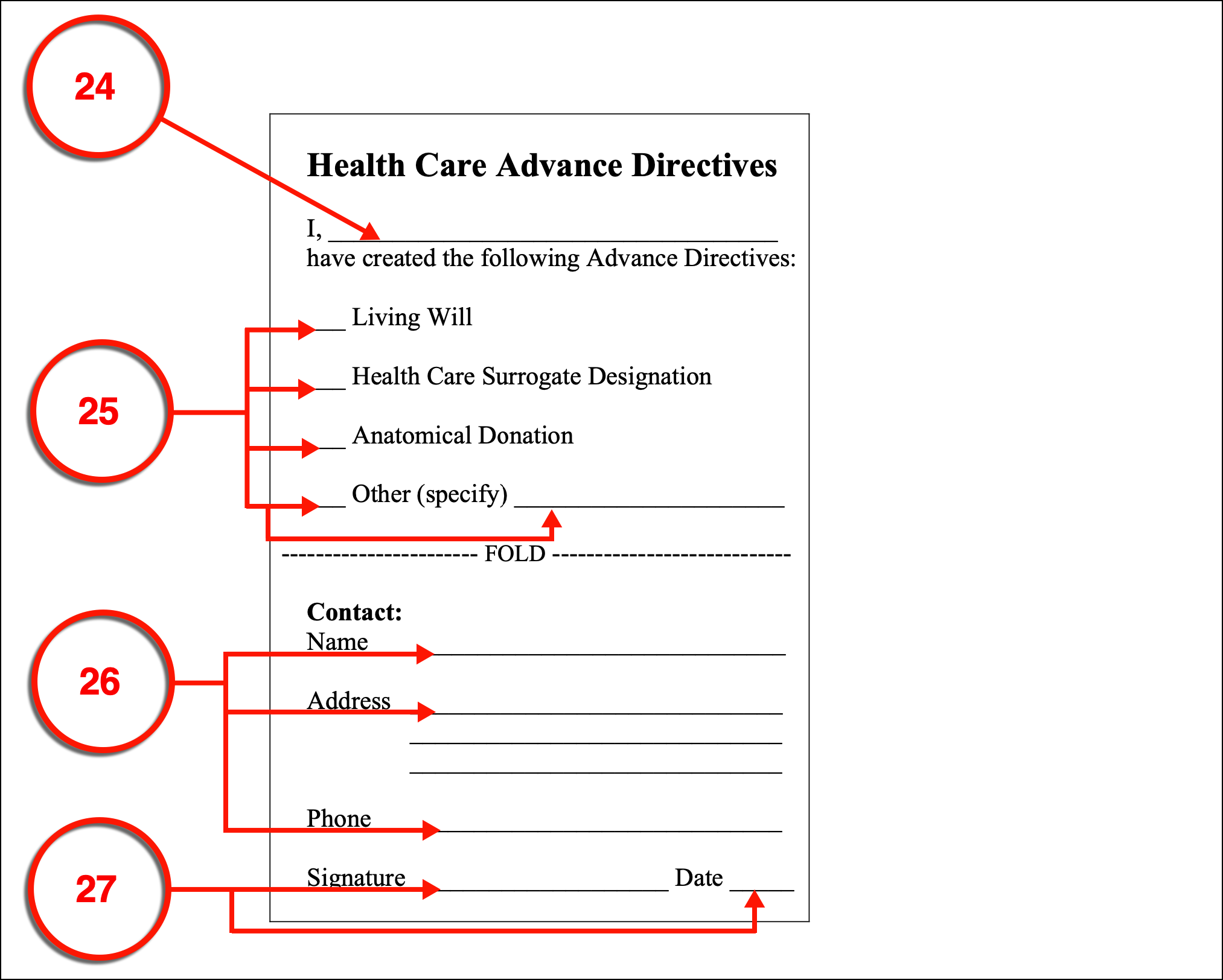
(24) Florida Declarant. A wallet card has been provided so that Emergency Responders who discover you unconscious and in need of medical aid can be made aware of your directive. To use this card properly, it must bear your full name.
(25) Directive Contents. Place a mark next to each form that you have filled out to convey your health care wishes. If needed you can utilize the area provided to list additional forms (i.e. Florida MOLST).
(26) Emergency Contact. Designating and recording the full name, address, and phone number of an Emergency Contact can aid Emergency Responders in assessing your medical condition and needs. This Party will be contacted through the information you record here to be informed that you have been found unable to communicate and in a serious medical condition. For example, Spouses or other Family Members are commonly listed as someone’s Emergency Contact.
(27) Validate The Wallet Card. To show Reviewers that you have intentionally reported this information, you must sign and date the completed wallet card before carrying it.Physician Orders For Life-Sustaining.
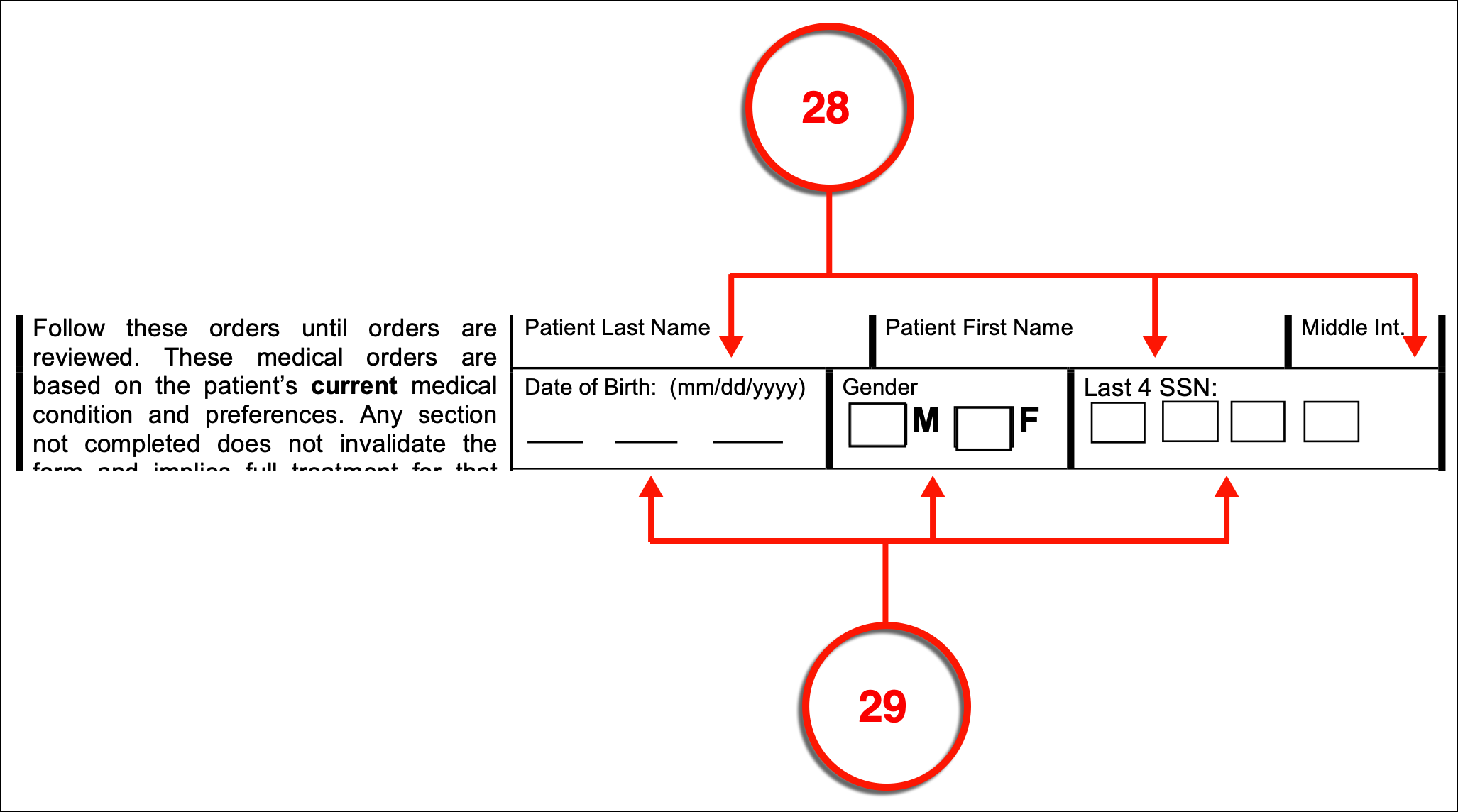
(28) Florida Patient Name. A valuable option this package provides is to include a Physician’s orders that support your treatment choices in your medical files. This form should be filled out with a licensed Physician (preferably licensed in the State of Florida) and will begin with a report on the Patient’s full name. Since this form can be filled out by a Physician, APR Nurse, or Physicians Assistant and the Patient’s legally appointed Health Care Surrogate or Representative, it is imperative that the full name of the Patient be easily found by Reviewing Medical Personnel.
(29) Supporting Information. The date of birth, gender, and the last four digits of the Patient’s social security number will aid future Reviewers in verifying the Patient’s identity.
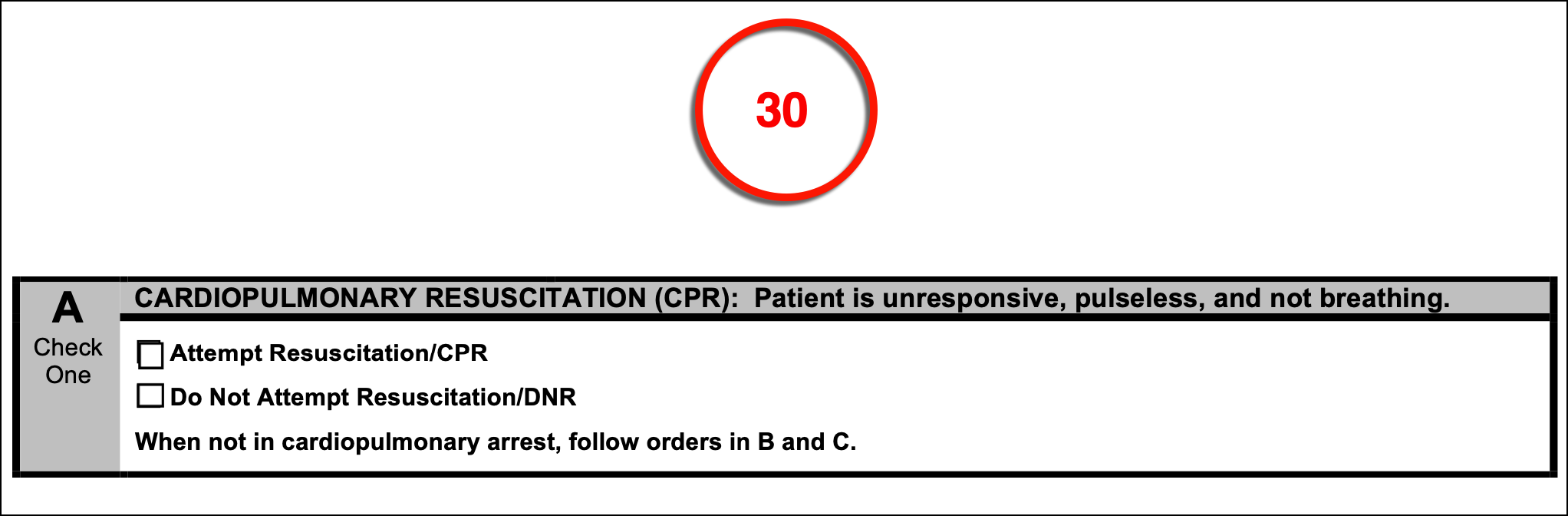
Cardiopulmonary Resuscitation (CPR)
(30) Florida CPR Directive. A key feature of the MOLST is its ability to quickly deliver the Florida Patient’s consent to receiving CPR or cardiopulmonary resuscitation when his or her hearts/lungs stop functioning or to deliver the Florida Patient’s refusal of this resuscitation technique.
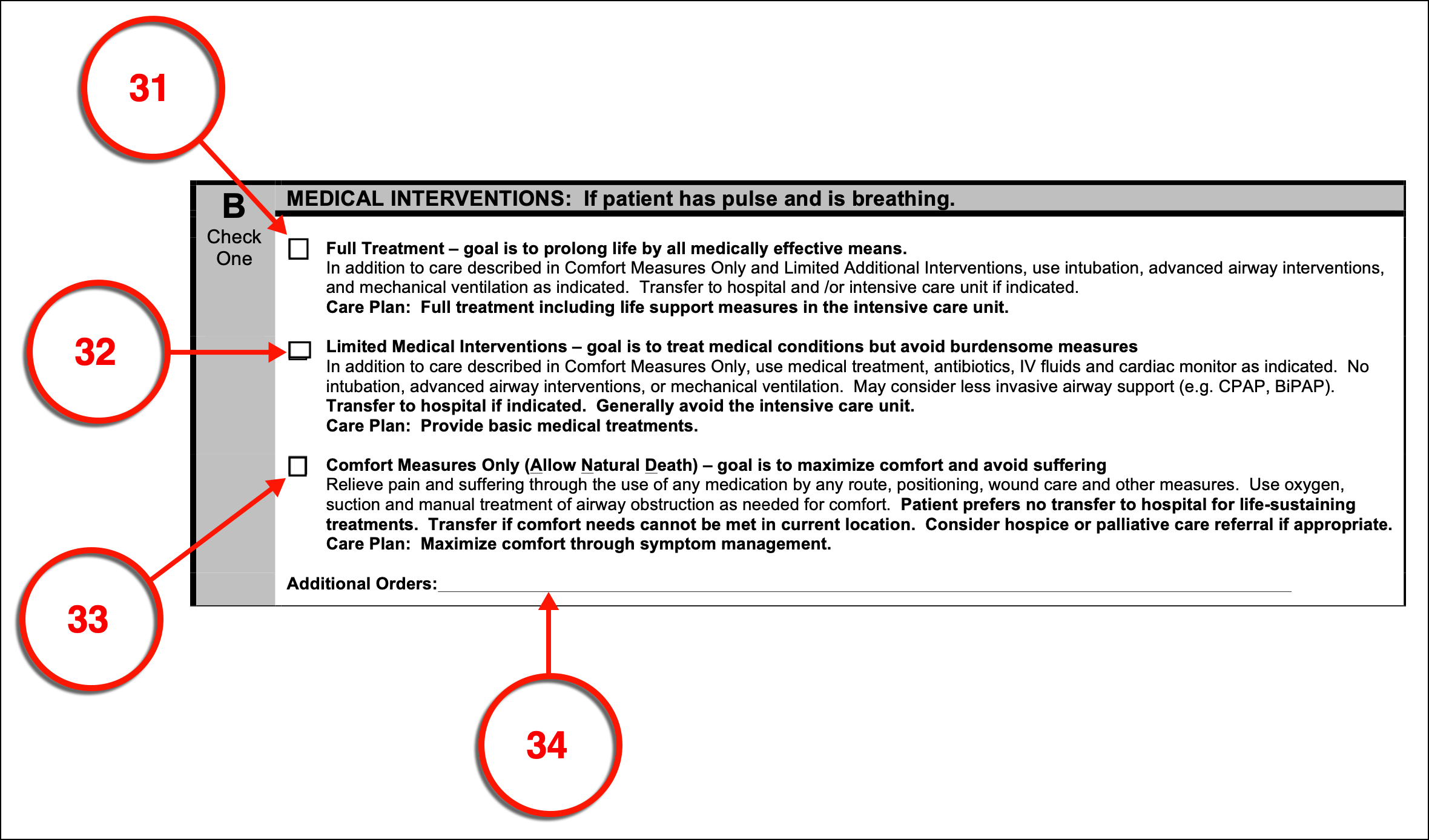
(31) Full Treatment In Florida. The level of treatment Emergency Personnel should use to respond to a medical condition that has incapacitated you but has left your hearts and lungs functioning can be determined with your Physician and recorded by selecting the appropriate checkbox statement. There are three levels to consider beginning with that of full treatment. If you wish to receive the full scope of treatment available to Florida Medical Responders (i.e. life support) then select the first option.
(32) Limited Medical Interventions. If desired, you may limit Florida Medical Responder’s medical intervention by selecting the second treatment option which allows for your medical condition to be treated without the use of “burdensome measures” such as intubation and mechanical ventilation (being attached to a breathing machine with a tube leading to your lungs. This will also instruct Florida Medical Responders to avoid the intensive care unit but give permission to admittance to a hospital for further treatment.
(33) Comfort Measure Only (Allow Natural Death). If you have determined with the agreement approval of your Physician that only comfort care should be employed by Florida Medical Responders if you are found incapacitated so that you may be allowed to die pain-free and comfortable (if possible) then select the final treatment description to issue this directive.
(34) Additional Orders. The final area where a discussion or instructions regarding the level of intervention you with Florida Medical Responders to assume as your treatment goal allows your entry of free form instructions. If you have any directions (i.e. you may wish a trial period of treatment), then consult with your Physician and record your medical preferences as needed.
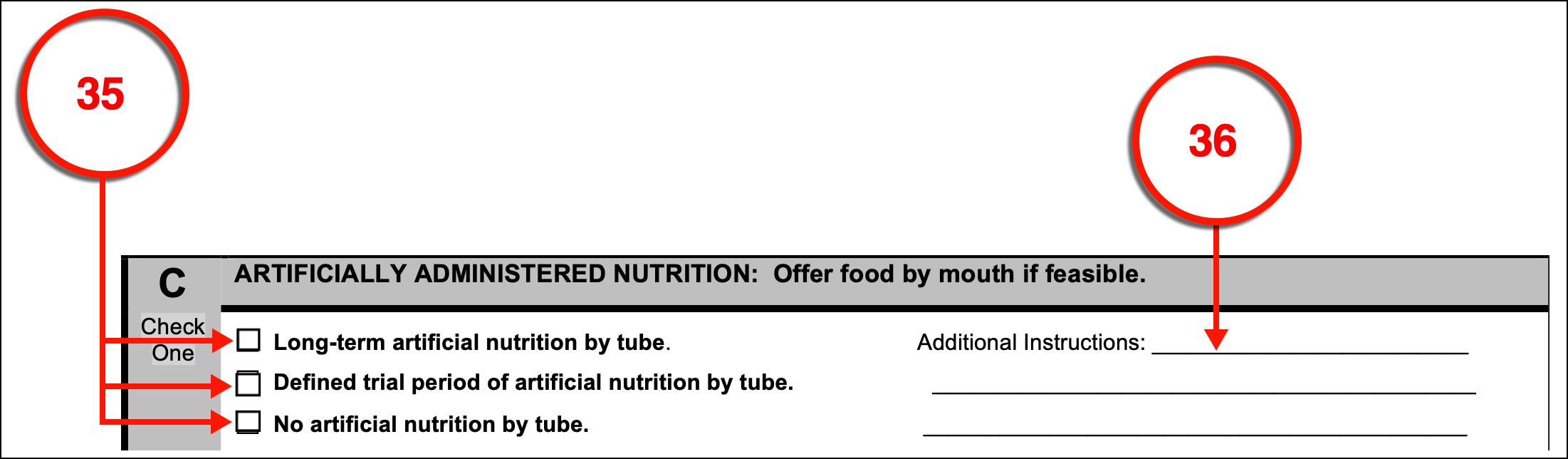
(35) Florida Nutrition Directive. In addition to medical intervention, a discussion on artificial nutrition is available. Here, you can define whether you will agree to artificial nutrition to be delivered by tube if it is necessary to keep you alive while you are incapacitated for an extended period of time if you will only consent to artificial nutrition delivered by tube for a limited amount of time, or if you refuse the administration of any artificial nutrition regardless of your medical condition, need for nourishment, and (anticipated) length of your incapacitation.
(36) Additional Instructions. As mentioned earlier, you can set a trial period on the administration of nourishment through a tube or intravenously. This trial period can be set to your preference you wish such as a medical event, a period of defined time, or to begin only under certain conditions. All such directives should be discussed with your Physician then reported in this area.
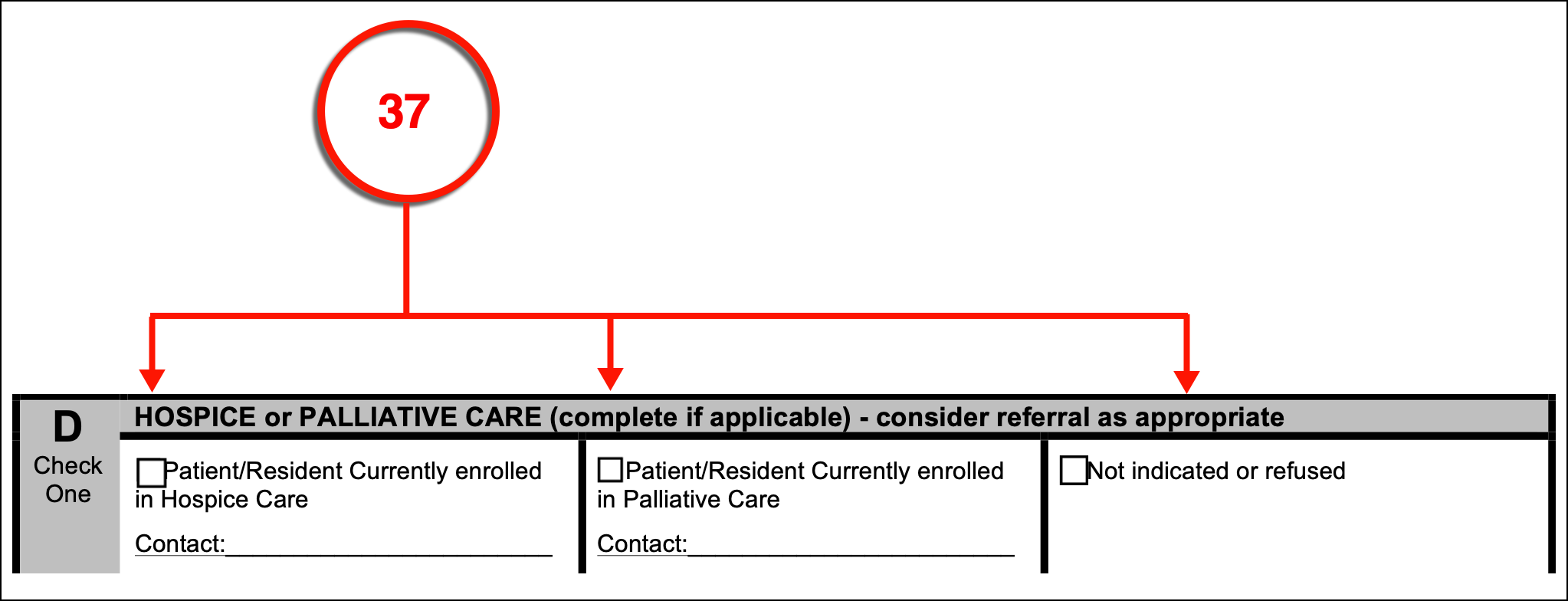
(37) Palliative Care Status. The status of the Florida Patient with hospice or advanced care institutions should be discussed. Thus, a section where it may be indicated if the Patient is enrolled in a Hospice Care Program that you list has been included along with a separate section where you can confirm the Patient’s enrollment in a Palliative Care Program that you name. If the status of the Florida Patient with such facilities is unknown, this too should be indicated by marking the appropriate checkbox.
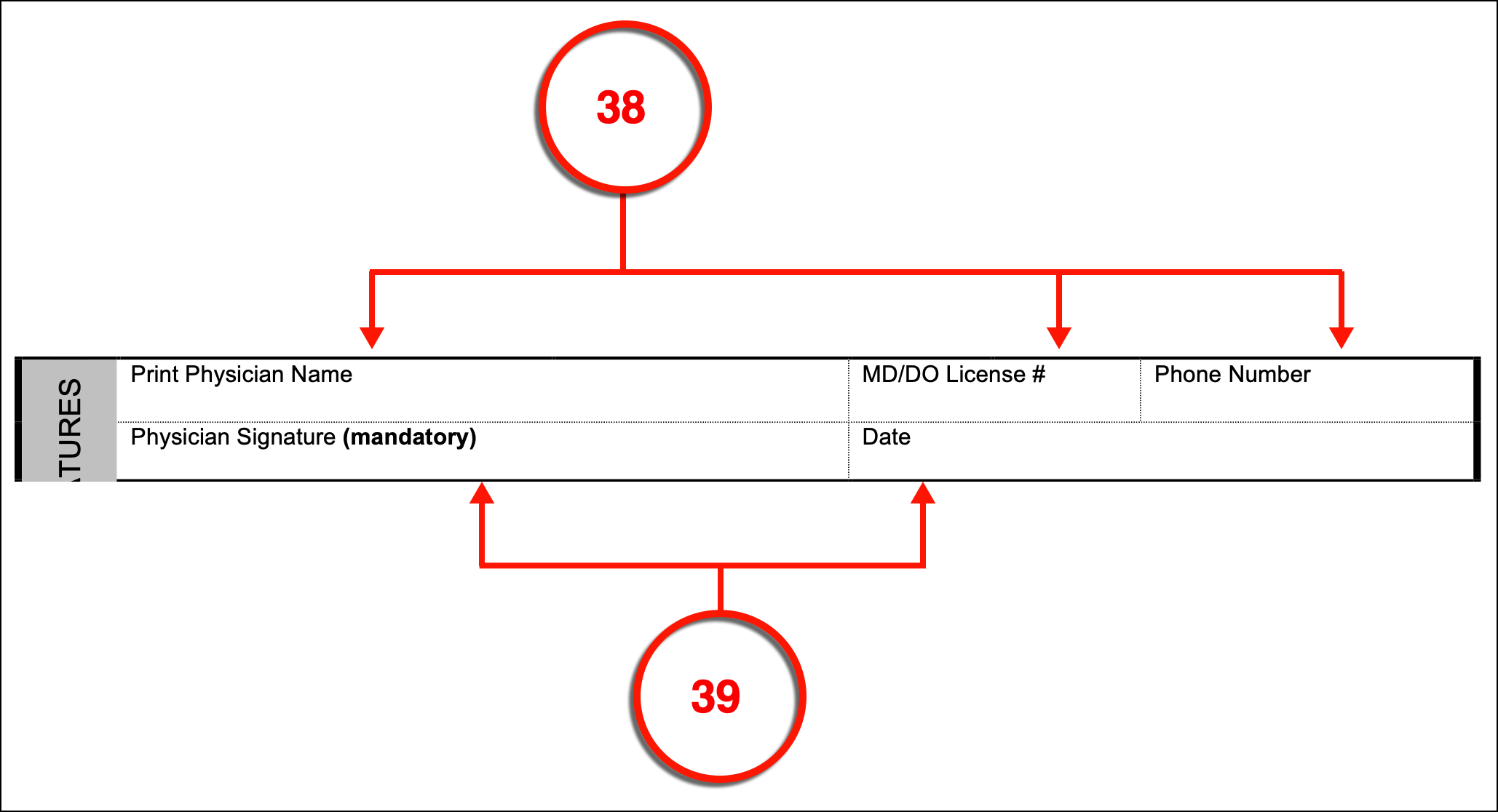
(38) Physician Florida MOLST Confirmation. The Physician who has completed this form with the Patient or the Patient’s Agent must furnish his or her printed name, MD/DO License #, and Phone Number.
(39) Physician Signature. The State of Florida makes it mandatory that this completed directive is signed by the Physician involved and that the date of his or her signature is reported.
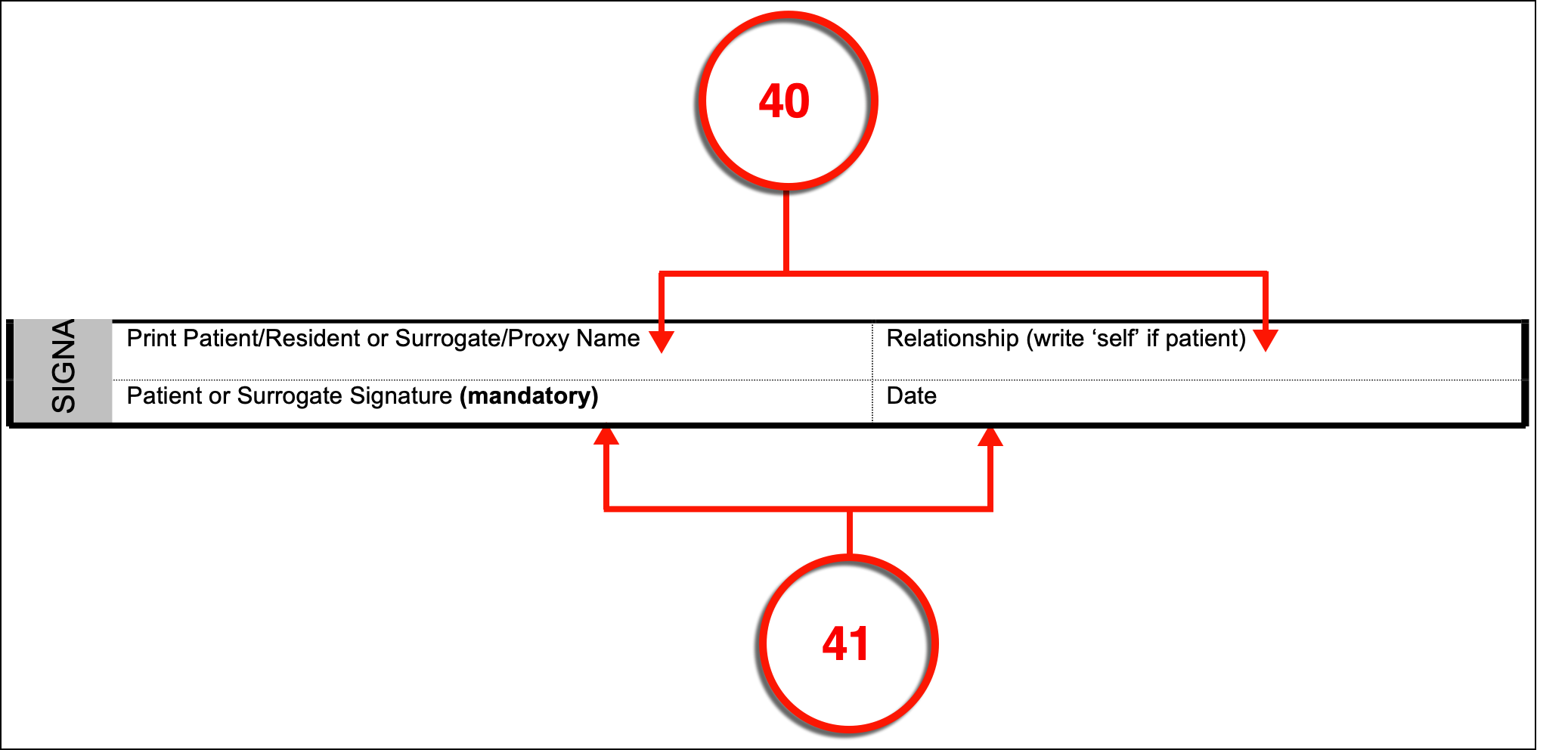
(40) Patient Or Surrogate/Proxy Identification. This paperwork can be filled out by the Florida Patient whose directives it conveys or the Florida Health Care Surrogate working on his or her behalf. The individual who has consulted with the above Physician to complete this form should print his or her name and discuss the relationship held with the Patient. If the Florida Patient has filled out this document personally, then the relationship held should be defined as “Self.”
(41) Florida Patient Or Surrogate Signature. The Florida Patient or Patient Surrogate identified as this form’s author must sign his or her name and provide the date when he or she completed this action.
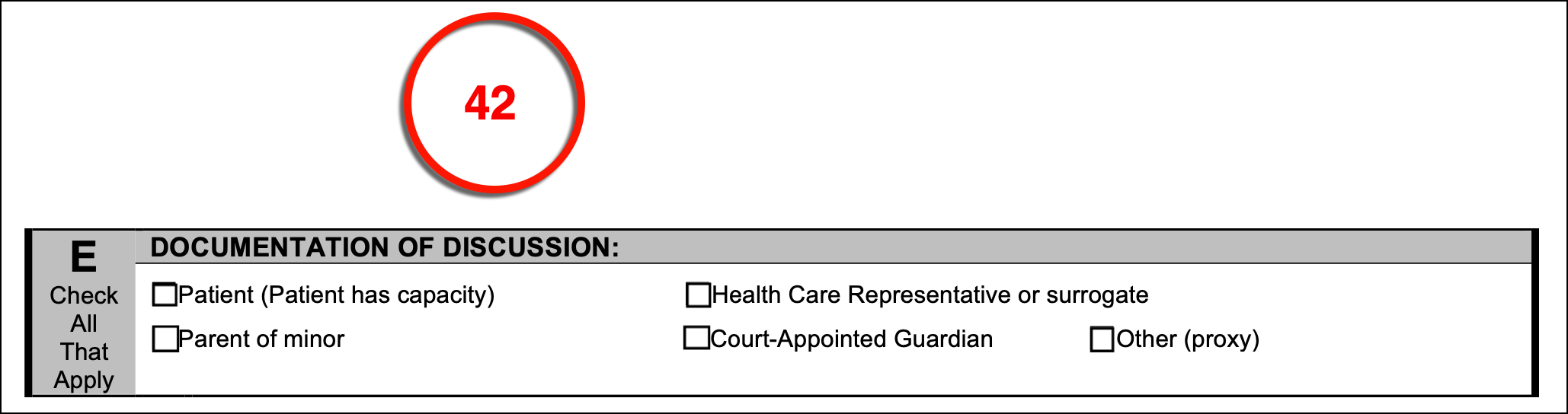
(42) Signature Declarant Status. The second page of the Florida MOLST contains the area needed to update its status in the Patient’s medical records however, it will also seek some additional reports beginning with exactly who the MOLST was completed by. A series of checkboxes allows an ideal method to identify if the Physician discussed the Patient’s medical care with the Patient, the Parent of the Patient (if the Patient is a Minor,), the Patient’s formally appointed Health Care Representative/Surrogate, or a Court-Appointed Guardian. If none of these definitions can accurately define the Proxy discussing the Florida Patient, then you may define this Party with a direct report to the appropriate area.
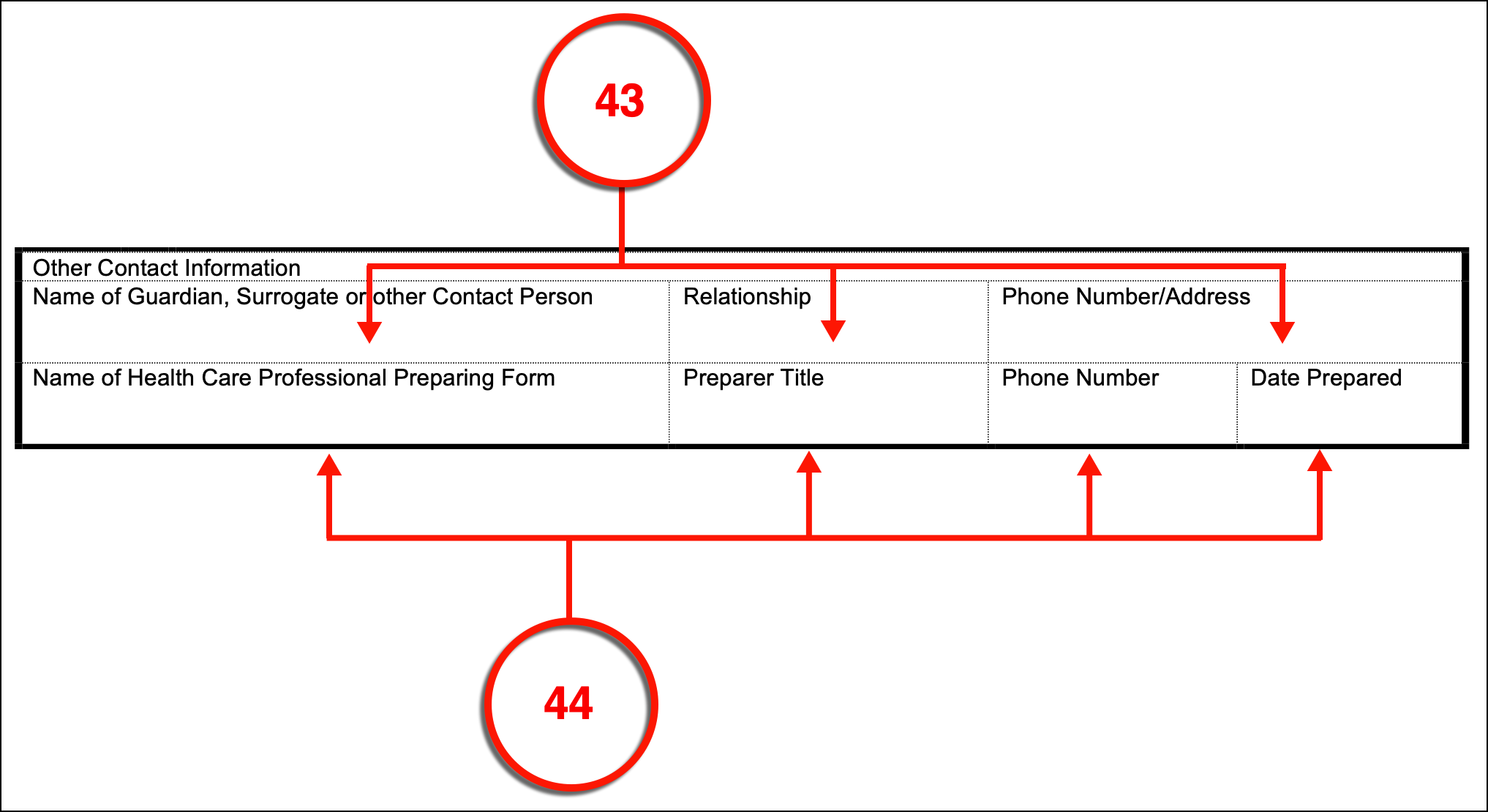
(43) Guardian , Surrogate Or Other Contact Person. To make sure the identities of those directly involved with the Florida Patient are solidified, record the full name of the Patient’s Guardian, Surrogate, or Emergency Contact, the relationship this Party holds with the Florida Patient, and the phone number needed to reach this Party.
(44) Health Care Professional Preparer. The Health Care Professional who has completed this form should also be identified by name, the official title he or she holds with the Medical Institution completing this form with the patient, the telephone number where this Preparer can be reached then the official date this document was completed by the Health Care Professional Preparer for the above Patient and Physician.
(45) Updating The POLST. In the future, Medical Personnel referring to this document will wish to make sure it is up-to-date and reflects the Physician-approved directives of the Florida Patient. To this end, a basic table where the date such a review takes place, the identity of the Reviewer, the institution where its status is discussed with the Patient or Surrogate can be provided. This information should be coupled with the formal status of this form as discovered from the Patient interview by marking the checkbox deeming it as unchanged, voided, or that a new MOLST has been issued.